The Top 10 Foot and Ankle Injuries in Soccer
Soccer is one of the most popular sports in the world, and one of the fastest-growing sports played by all ages. There is a tremendous amount of stress placed on the player’s lower extremity requiring excessive running, side-to-side movements, and starting/stopping, resulting in foot and ankle injuries. Injuries occur which can be traumatic or acute or caused by overuse. With the men’s World Cup around the corner this year I’ve come up with a top 10 list of foot and ankle injuries in soccer. This list is comprised of several years of treating professional, collegiate, high school, and recreational soccer players. There are probably other injuries that I’ve excluded but these are the most common ones I have seen.
BLISTERS
Blisters may be one of the most common skin disorders seen. These are small bubbles on the skin filled with fluid caused by skin shear. Depending where located on the foot, they may or may not be painful. If not treated properly, complications such as cellulitis, or infection can occur. Blisters happen when there is a tear between the top three layers of skin with fluid buildup. Moisture and skin temperature are common causes of the shearing forces that create blisters. Blisters should be drained immediately using multiple puncture sites with care to preserve the roof or skin of the blister. Removal of the roof can result in more pain and an increased risk of infection. If you need to return to activity immediately, then some type of topical antibiotic or gel is effective. Engo blister patches are a very effective way to prevent recurring blisters. Other reported methods of blister prevention include Vaseline, antiperspirants, and moleskin although studies don’t support the use of these.

SUBUNGUAL HEMATOMA/BLACK TOENAIL
Soccer players and runners seem to have the most frequency of black toenails. Because of a shoe that is too short or too long, there is trauma to the toenail resulting in blood accumulating under the toenails. The blood will dry and attach to the
underside of the nail thus the purple or black discoloration. Depending how much nail is involved determines if you will lose the nail or not. If greater than >50% of the nail is involved this usually means the nail will come off. If less than 50% of nail involvement,
a new nail will likely grow out pushing the damaged nail off. If painful at the time of injury, then the best treatment is to have the area drained so as not to affect training and games. Oftentimes, medical professionals can, or will drain the toenail, otherwise if not painful they can leave the nail untouched. Occasionally, the nail may need to be removed.

TURF TOE
Turf toe is a common condition of the big toe joint in athletes requiring push-off when running or a change of direction. It commonly occurs when the toe is bent too far (sprained), stretching and injuring the tendons and ligaments around the joint. While more common with players playing on turf, it can occur on other playing surfaces. Treatment should focus on rest, ice, non-steroidal anti-inflammatories, shoe modifications, splinting or taping, immobilization in a boot, and occasionally surgery. This can be a very debilitating injury if not treated immediately, and non-treatment leads to chronic changes.
ANKLE SPRAINS
Ankle sprains are the most common soccer injury in the lower extremity. An ankle sprain occurs when ligaments that support the ankle stretch beyond their limits and tear. The severity of a sprain can vary greatly depending on the number of ligaments and the extent to which the ligaments are torn. Most ankle sprains heal with conservative treatments like ice, elevation, compression, and protection. If your ankle remains swollen or painful for several weeks despite conservative treatments, you may need additional testing to check if you have a torn tendon, ligament, or other fracture. If symptoms do not improve despite non-operative treatment, you may need surgery to repair or reconstruct the injured ligaments. Without proper treatment and rehabilitation, an untreated ankle sprain can weaken your ankle, making it more likely that you will
reinjure it. Athletes with chronic ankle sprains can end up with chronic ankle pain, instability, and even arthritis. Newer advanced technology like MLS laser can reduce swelling and pain resulting in a quicker recovery.
MIDFOOT SPRAINS
The midfoot portion of your foot serves to support and stabilize the arch of your foot. This area of your foot is a cluster of bones and ligaments that have very tight connections to each other. When an injury occurs, it can affect the ligaments, bones, or cartilage of the tightly fitted joints. There are three basic types of injuries that occur at the midfoot: sprain, fracture, or dislocation. Midfoot sprains, or LisFranc’s injuries, can be one of the most debilitating injuries and take the longest to recover from in this list of 10 injuries. A midfoot sprain affects the ligaments and soft tissue across the middle of the foot after a poorly attempted tackle, being stepped on, excessive cutting, or twisting motion. Persistent swelling, pain, and bruising are symptoms that shouldn’t be ignored. Midfoot sprains should be thoroughly evaluated. X-rays are often negative so additional imaging like an MRI is usually necessary. Based on the severity of the injury, treatment can vary. Initial treatment should focus on addressing the pain and inflammation, and usually, a walking boot is necessary and occasionally non-weightbearing with crutches. I have seen some midfoot sprains take months to heal. If a fracture does occur, then surgery is usually needed otherwise there are long-term complications.
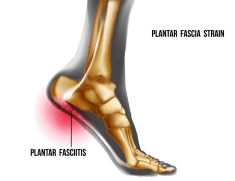
PLANTAR FASCIITIS
One of the most common foot injuries in sports is plantar fasciitis. Typically this is an overuse injury that occurs because of strain on the thick ligament on the bottom of the foot, the plantar fascia. Pain can be located in the heel or arch, and oftentimes is associated with a heel spur. Characterized by first-step pain when getting up in the
morning or after sitting for a while, usually, the pain will ease after a few minutes and can get worse later in the day. A good analogy is if you stretch a rubberband, over time it will eventually give and that’s what happens to the plantar fascia. Because of the constant tension put on the plantar fascia with the constant running required by soccer, if not treated immediately or effectively, the injury could rapidly result in loss of time on the pitch. Treatment options consist of ice, non-steroidal anti-inflammatories, stretching, night splints, steroid injections, orthotics, shockwave therapy, and surgery.
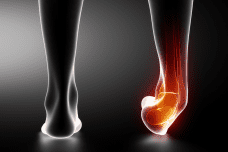
ACHILLES TENDONITIS
Achilles tendonitis is a common acute or overuse condition that occurs when the large tendon that runs down the back of the lower leg becomes irritated and inflamed. The Achilles tendon can become inflamed where it attaches to the heel bone (insertional) or it can be inflamed above the tendon insertion (non-insertional). When the tendon is inflamed for a long period of type, the condition is often referred to as Achilles tendinopathy. Achilles tendonitis or tendinopathy can be a precursor to an Achilles tendon rupture. Causes of Achilles tendonitis include tight calf muscles, shoe irritation, or a change in activity that causes repetitive stress to the tendon. Symptoms include pain and stiffness in the morning, pain with activity, a bump on the back of the heel bone, and pain with irritation from the shoe. X-rays can help determine if a bone spur is present, and an MRI may be needed if the pain isn’t getting better. Treatment consists of rest, ice, NSAID’s, physical therapy, heel lifts, night splints, orthotics, stretching, and shockwave therapy. Modifications to the heel counter of the shoe can also be effective. Cortisone injections are not used in the treatment of Achilles tendonitis as they can cause the tendon to tear. In some cases, if a bone spur is present, surgery may be necessary so all options should be exhausted before reaching that point.
5TH METATARSAL FRACTURES
Because of the constant starting, stopping, and cutting required in soccer, another serious injury is 5th metatarsal fractures. Famous soccer players like David Beckham, Wayne Rooney, and Neymar all suffered from some form of a 5th metatarsal fracture. These can be divided into stress fractures, avulsion fractures, and Jones fractures. Stress fractures are a result of increased torsional forces on the bone and there is increased swelling in pain. Avulsion and Jones fractures are a result of an acute injury, likely an ankle sprain but in these cases, the tendon that attaches to the 5th metatarsal pulls a piece of bone off. Jones fractures can be the most serious because the fracture interrupts the blood flow to the bone. Jones fractures often require non-weight bearing in a cast or even surgery to insert a screw.
CALCANEAL APOPHYSITIS
Heel pain in children is one of the most common, and under-diagnosed conditions, especially in soccer. If there has been no injury, and your child limps during or after practice or games, there’s a good chance he/she has calcaneal apophysitis or Sever’s disease. The growth plate in the heel bone is irritated from impact and stress from the soft tissue attachments. This condition is most commonly seen in kids from the ages of 8-14. Typically, there is pain with activity and relief with rest, and rarely is there swelling or bruising. Treatment consists of rest, ice, NSAID’s, heel lifts, orthotics, and immobilization. I’ve had really good success with custom orthotics with a very specific prescription that has been effective for about 90% of my kids.
SHIN SPLINTS
Shin splints can be troubling for athletes and cause considerable frustration and downtime. While there are multiple reasons one can have shin pain; shin splints, or medically called medial tibial stress syndrome (MTSS), is one of the most common leg injuries seen in athletes. The cause of these isn’t well understood, and there are many different treatment options, which very few have been validated in the literature. Usually, pain is a dull, aching pain along the tibia or leg bone. Early in the process, pain may start at the beginning of training, improves throughout the activity, then increases towards the end. As the condition progresses, the pain may become more constant. Often, the pain goes away with rest until the activity is started again the next day. Rarely is there swelling, and if there is, there may be a more serious issue than shin splints. A tibial stress fracture can present very similar to shin splints, but the pain is more localized than up and down the bone. Pain at night isn’t unusual in a stress fracture. X-rays are usually negative in a stress fracture so an MRI may be necessary to determine the difference.
Many different variables contribute to the development of shin splints. Risk factors for shin splints can be classified as activity related or biomechanical. Activity-related risk factors include abrupt changes in training, training on hard surfaces, inadequate arch
support, and poor athletic footwear. Biomechanical causes include excessive pronation of the foot in combination with repetitive impact activity. Females are more likely to develop shin splints than men. There are multiple treatment options for shin splints, but realistically, there isn’t much science to support them. The primary management of shin splints in an ideal world is rest, but that isn’t always practical for an athlete who is unable to take time off and cross-training must be a consideration in those instances. These activities should be performed in a manner that limits stress on the tibia. Ice and ice massage may be used acutely to reduce swelling and inflammation. NSAIDs are appropriate for pain relief. Stretching programs for the calf and hamstrings may be helpful for cases in which these muscles are excessively tight. Physical therapy modalities including ultrasound, iontophoresis, electrical stimulation, and massage, may be beneficial. If biomechanical abnormalities are the cause, then those should be addressed with the use of orthotics. A compression sleeve may provide some relief. In my years of treating shin splints, I have found custom foot orthotics with a very specific prescription to be very, very useful in resolving shin splints. In addition to orthotics, I have found massage, ice, and a compression sleeve to help reduce the pain. More recent advances in treatment is shockwave therapy, and this has been proven to be very helpful.
If you suffer from any of these above conditions and aren’t getting better, telemedicine consults are available through the Colorado Center of Pediatric Sports Medicine or call (720) 600-3380 to make an appointment so your pain can be resolved.
Visit Us
1551 Professional Lane, Ste. 105
Longmont, CO 80501
Contact us
(720) 600-3380 Tel
(720) 306-5430 Fax
Hours
By Appointment Only
Servicing Communities Along the Front Range and Beyond
© Colorado Center for Podiatric Sports Medicine | Privacy Policy

